Losing a pregnancy is an emotionally overwhelming experience, and for many families, the biggest question that follows is “why did this happen?” A fetal autopsy can provide important answers. By carefully examining the baby, placenta, and sometimes conducting genetic studies, doctors can identify the underlying cause—whether it’s due to genetic abnormalities, infections, placental issues, or maternal health factors. These findings are not only crucial for closure but also guide medical teams in planning safer, healthier future pregnancies. Understanding how fetal autopsy helps prevent recurrence can empower parents with knowledge and provide reassurance for the journey ahead.
What is a Fetal Autopsy?
A fetal autopsy is a detailed post-mortem examination of the baby, placenta, and sometimes other tissues. It is carried out after a miscarriage, stillbirth, intrauterine death, or pregnancy termination.
This examination can:
- Provide a clear or partial explanation for pregnancy loss.
- Offer a specific medical diagnosis that may differ from or add to the clinical diagnosis.
- Help in understanding genetic and structural abnormalities by linking physical features (phenotypes) with underlying genetic causes.
- Play a vital role in assessing recurrence risk in future pregnancies.
In short, fetal autopsy is not just about finding the cause of loss, it also bridges clinical care with modern genetic insights, guiding parents and doctors toward better future outcomes.
Why is Fetal Autopsy Important?
Fetal autopsy is considered the gold standard diagnostic tool when it comes to understanding why a pregnancy ended in miscarriage, stillbirth, or intrauterine death. It helps doctors uncover the immediate cause as well as contributing factors that may not have been apparent during pregnancy.
One of its most valuable roles is in identifying underlying diseases or conditions such as fetal growth restriction, congenital malformations, maternal diabetes, or genetic disorders. These findings are not only important for explaining the past, but also for predicting the recurrence risk in future pregnancies. This allows clinicians to give parents accurate counselling and prepare targeted care plans.
Beyond individual families, fetal autopsies also add value to public health systems by contributing to congenital anomaly registries, clinical review meetings, and audits of antenatal and intrapartum care. In this way, they improve both personal and community-level pregnancy outcomes.
Benefits of Fetal Autopsy
Fetal autopsy is a valuable tool that goes beyond simply confirming a cause of pregnancy loss. Its benefits include:
- Ascertain the cause of death
- Corroborate, supplement, or refute clinical diagnosis
- Evaluate diagnosis and therapy, including new modalities
- Identify rare diseases
- Detect and discover new pathologic entities
- Document hitherto unknown information on disease manifestations
- Document growth and development
- Provide risk estimates for future pregnancy
- Further the cause of research and education
- Facilitate the investigation of environmental, occupational, and lifestyle causes of diseases
- Provide epidemiologic data
- Provide organs for donation and study
- Bereavement closure
Key Insights of Foetal Autopsy:
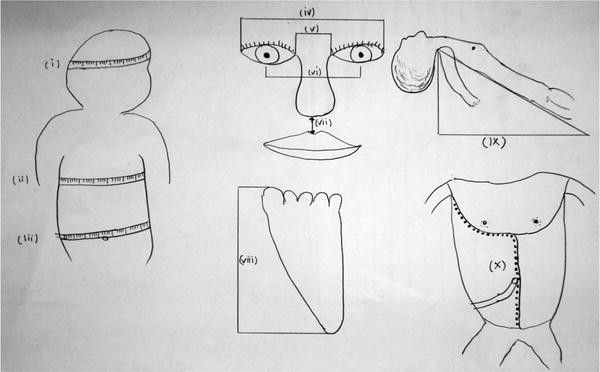
Perinatal autopsy provides detailed information about the fetus and placenta, helping doctors understand the cause and timing of intrauterine death. It evaluates:
- Fetal growth and maturity: By measuring body and organ weights and bone lengths and examining ossification centres, autopsy determines if growth is appropriate for gestational age and assesses fetal maturity.
- Congenital anomalies: Identifies structural abnormalities and variations from normal development and helps in differential diagnosis of syndromes or sequences.
- Fetal stress and anaemia: Detects signs of fetal stress, growth restriction (e.g., elevated brain-to-liver ratio), or anaemia.
- Infections: Uses gross, histologic, microbiologic, and molecular analyses to detect infections.
- Placental and umbilical cord pathology: Evaluates placental insufficiency, vascular obstruction, thrombosis, infarction, or cord abnormalities, which may explain stillbirth or preterm delivery.
- Inherited and immune-related risks: Detects conditions like thrombophilia or antiphospholipid antibodies that affect placental function and fetal outcomes.
Final Thoughts:
Fetal autopsy is more than a medical procedure it is a powerful tool for understanding pregnancy loss, guiding future care, and providing emotional closure. It allows clinicians to offer accurate counselling, assess recurrence risks, and plan safer pregnancies. Beyond individual families, fetal autopsies contribute to research, public health data, and medical education, bridging clinical care with modern genetic insights. Ultimately, opting for a fetal autopsy empowers parents with knowledge, supports informed decisions for future pregnancies, and strengthens overall prenatal care, turning a tragic event into an opportunity for learning and reassurance. LifeCell Diagnostics provides comprehensive fetal autopsy services, offering families genetic insights and expert analysis to understand pregnancy loss and plan safer future pregnancies.